With rigorous advancement in science and technology, ICSI infertility treatments have become available to couples, regardless of whether they are of the same gender or opposite, aiming to conceive a baby.
According to the World health organization, 25% of India suffers from infertility problems yearly.
The reasons for infertility may be a poor lifestyle, hormonal imbalance, genetic problems, or any other condition that cannot be cured.
To cure the same, ICSI, IVF, IUI, and other infertility treatments are adopted by gynecologists and other IVF specialists to deliver the happiness of having an extended family.
In this blog, we will deep dive into what the term Intracytoplasmic sperm injection means, the process, success rates, the risk involved, and when there is a need.
Let’s get started!
What is ICSI?
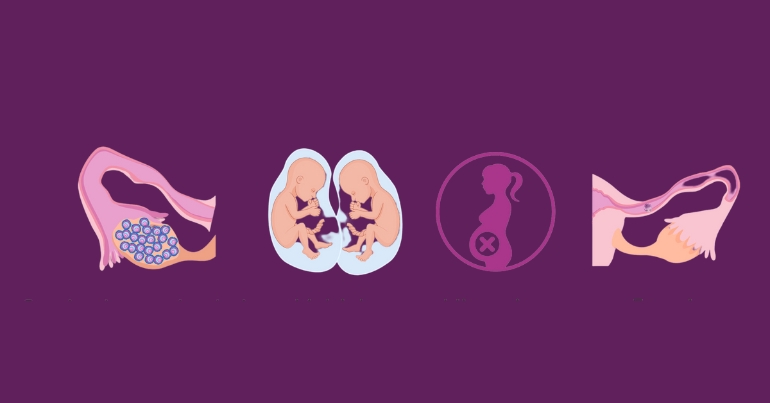
ICSI, or Intracytoplasmic sperm injection, is an infertility treatment that involves the injection of live sperm directly into a person’s egg in a laboratory, resulting in the creation of a fertilized egg.
There are higher chances of failure in ICSI due to the possibility of the sperm failing to fertilize the eggs.
Intracytoplasmic sperm injection is mostly used when there is a problem in conceiving a baby due to male infertility reasons. These male infertility factors include low sperm count, reduced motility, erectile issues, and azoospermia with no identifiable cause.
What is the ICSI Process?
1. Sperm Retrieval
The initial step of the ICSI process begins with collecting a sperm sample, either through ejaculation into a cup or surgically retrieved. Subsequently, mature eggs are retrieved from the ovaries of the female partner. This egg retrieval procedure uses a minimally invasive procedure called egg retrieval.
During this step, ultrasound guidance is employed to locate and aspirate the fluid-filled follicles containing the egg.
2. Injection of Sperm into Egg
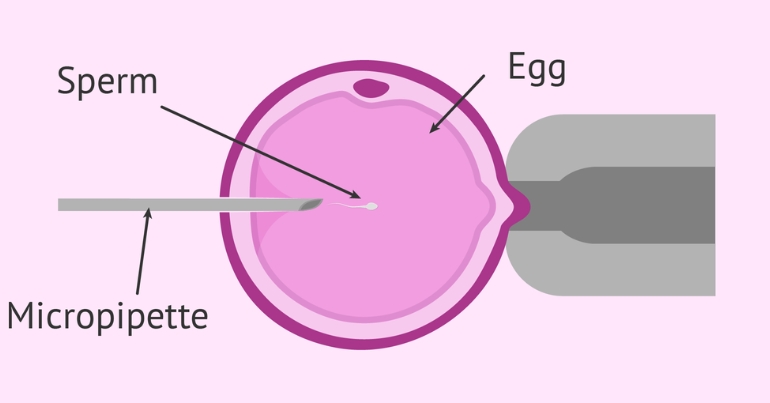
After the egg retrieval procedure, a healthy sperm is selected for injection. This sperm can be obtained from male partners’ ejaculated semen or sperm donor. If the male partner has limited sperm count, poor motility, or abnormal morphology, a single viable is chosen under a high-powered microscope.
An embryologist then uses a specialized needle to inject the chosen sperm into the mature egg cytoplasm delicately.
3. Monitoring the Embryo
After the injection, the fertilized egg is closely monitored for signs of successful fertilization. This ICSI process involves observing the zygote’s development and cell division under controlled laboratory conditions. Over time, the zygote progressed through various stages, eventually forming an embryo.
4. Transfer of Embryo
After a period of growth and development, only the most viable embryos are selected for transfer into the woman’s uterus. The cycle occurs 3 to 5 days after fertilization. The number of embryos transferred is determined by factors such as the woman’s age, the quality of embryos, or any ICSI attempts.
The ultimate goal of embryo transfer is to achieve successful implantation within the uterine lining and achieve a pregnancy.
At Nimaaya, our ICSI fertility specialist conducts a consultation session for couples adopting the ICSI process to conceive a baby. We make sure that all the risks, side effects, and other problems are solved before moving further and making it successful.
Also Read: Understanding the ICSI Procedure: Step-by-Step Guide to Assisted Reproductive Technology
When is there a need for ICSI?
• IVF was not Successful
When traditional fertilization methods like IVF were unsuccessful, techniques like ICSI were adopted. ICSI involves directly injecting sperm into an egg, increasing the likelihood of successful fertilization.
Also Read: ICSI vs IVF: Difference Between Fertility Treatment Options
• Advanced Maternal Age
As we saw in the last blog on IUI, the age of a woman can affect the quality of her eggs and ultimately lead to the chances of fertilization. In this case, where the female partner is over 35, the IVF specialist adopts ICSI. This method enhances the chances of fertilization by passing potential age-related barriers.
• Using Previously Frozen Eggs
Frozen eggs generally exhibit lower survival rates compared to fresh eggs. ICSI comes into play when optimizing frozen eggs, addressing the challenges associated with the freezing process, and increasing the chances of successful fertilization.
• Low or Poor Sperm Quality
In the case of male infertility characterized by problems like low sperm count and poor sperm quality, conventional fertilization methods may not yield successful outcomes. On the other hand, ICSI should be used as it involves directly injecting a single viable sperm into the egg.
• Blockage in the Reproductive System
There might be chances of blockage in the male reproductive system that prevents the release of sperm during ejaculation. The condition can be overcome with ICSI because sperm can be directly retrieved from the reproductive tract, which can be used for injection into the eggs.
• Inability to Ejaculate
When the male partner faces challenges in ejaculating or producing adequate sperm for fertilization, ICSI sperm preparation becomes the ultimate solution. Sperm can be collected through procedures like TESA and TESE and subsequently utilized for injections.
Risk of ICSI
While ICSI has proven to be the most effective in achieving successful pregnancies, it’s essential to acknowledge the potential risk associated with procedures such as:
• Embryo Damage
The mechanical manipulation in transferring eggs and sperm during the ICSI cycle has a higher chance of causing potential embryo damage. This damage will affect the embryo’s viability and development stages.
• Multiple Pregnancies
ICSI increases the likelihood of multiple pregnancies, which can lead to complications for both the mother and babies. Complications issues like low birth weight, and gestational diabetes, demand heightened medical attention and care.
• Sperm Quality and Selection
The success of ICSI, as well as other fertility treatments, depends upon selecting a healthy sperm. This selection process significantly contributes to a couple’s ability to conceive. Even a minor variation in sperm quality could lead to the detection of genetic abnormalities, directly affecting the embryo’s health.
• Birth Defects
When couples opt for the ICSI process increases the chances of getting congenital disabilities in children. These defects could be because of the parent’s genetics, sperm quality, or any other unpredictable risk that might be detected later.
ICSI Success Rate
According to the American Society for Reproductive Medicine (ASRM), the chances of ICSI fertilizing eggs are between 50% to 80%.
This is because in ICSI, eggs don’t always result in developing viable embryos, or the chances of eggs during the process can be damaged. Also, there are chances that the embryos don’t grow themselves.
At Nimaaya, our dedicated team of ICSI specialists consistently achieves milestones in accomplishing the success rate and bringing joy to millions of families.
There might be multiple factors that affect the success factors of ICSI. Let’s explore them in detail:
Factors that Affect the Success Rate:
ICSI success rate is affected by several factors, often varying between couples. But to put it in a nutshell, a few factors will collectively influence the outcome of success rate:
• Female Age
Just like other infertility treatments, the success of ICSI is also affected by women’s age. This means younger women have higher success rates due to healthier and higher-quality eggs.
• Male Factor Infertility
ICSI male infertility constitutes a significant factor affecting ICSI success rates. The quality, quantity, and motility of sperm are crucial determinants. If these factors are compromised, the likelihood of ICSI failure increases.
• Embryo Quality
The quality of embryos plays a significant role in the successful completion of the ICSI process. If not, then the successful implementation and chances of successful delivery get reduced.
• Number of Embryos Transferred
The number of embryos transferred after each ICSI cycle requires careful monitoring. At Nimaaya, the team observes the quality and quantity of embryos transferred. Excessive embryo transfer can elevate the risk of multiple pregnancies and related complications.
Is ICSI Procedure Painful?
No, the ICSI procedure from retrieval to transfer of embryo is not at all painful. Because of other fertility treatments, there has been a myth that ICSI is also painful.
There are only two steps in the whole procedure:
Firstly, the patient is given an injection just like insulin. Secondly, the patient is given general anesthesia during egg pick-up.
To conclude, one can easily pass all the process steps without experiencing any pain.
Key Takeaways
To sum up, we learned that besides choosing IVF fertility treatment there are also other fertility treatments that one can go for.
ICSI over any other treatment because it is not painful, involves easy steps in the procedure involved, and has more success chances as compared to IVF.
If you and your partner consider adopting the ICSI process, you can begin your journey with one of the best fertility treatments across Gujarat, Nimaaya.
You can trust us! Your dream to expand your family will be successful with our specialists, Dr. Pooja Nadkarni Singh, and Dr. Yuvrajsingh Jadeja. Their guidance guarantees a smooth ICSI or any other fertility treatment journey.
With over 30 years of experience in the field, Nimaaya stands with you at each stage of your fertility treatment. Our dedicated team will support you with updated technology and help you successfully conceive a baby without any complexions. Book an appointment with Nimaaya today and get on your path to parenthood with confidence.