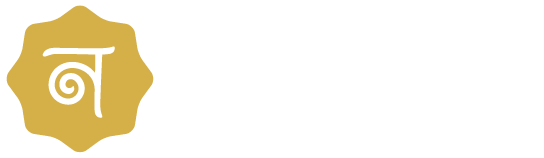
Early Detection of Ectopic Pregnancy: A Detailed Guide
Ectopic pregnancy is a medical and potentially fatal condition characterized by extramural implantation of a fertilized ovum, and the fallopian tube is usually the site of implantation. Ectopic pregnancy needs to be diagnosed at the earliest possible moment to prevent complications and to receive treatment.
Symptoms suggestive of an ectopic pregnancy could be abdominal pain, vaginal bleeding, and/or shoulder pain. If there is no early intervention, the condition may result in the rupture of the fallopian tube, which may cause a major internal haemorrhage.
This guide will discuss the various approaches, symptoms, and diagnostic tools in preventive strategies for the early detection of ectopic pregnancy.
What is ectopic pregnancy
Ectopic pregnancy accounts for about 1-2% of all pregnancies. The majority occur in the fallopian tube (tubal pregnancies), though they may occur in the cervix, ovary, abdominal cavity, or at sites of previous cesarean section scars.
Possible symptoms of ectopic pregnancy include abdominal pain, vaginal bleeding, and, in some cases, shoulder pain. Untreated, ectopic pregnancy can be life-threatening, demanding immediate medical attention.
People Also Search: Ectopic Pregnancy in Hindi
Why Does Ectopic Pregnancy Happen?
An ectopic pregnancy has usually occurred as a result of any obstruction that prevents the fertilized egg from travelling to the uterus. The conditions responsible for its occurrence include:
Pelvic inflammatory disease (PID):
The infection may encourage scarring in the fallopian tube due to infection by chlamydia or gonorrhoea, thus preventing the fertilized egg from reaching the uterus, resulting in ectopic pregnancy. Other risk factors for ectopic pregnancy involve a history of previous ectopic pregnancies, a history of infertility in a woman, and forms of contraception such as tubal ligation.
Previous ectopic pregnancy:
Previous history of ectopic pregnancy increases risk for women. They may also be more prone to ectopic pregnancies if they’ve had a tubal ligation or a history of infertility. Individuals fitting into these risk factors should therefore seek medical attention as soon as possible in case of suspicion for ectopic pregnancy.
Tubal surgery or abnormalities:
Procedures to reverse tubal ligation and conditions such as endometriosis also increase the risk. Other general factors are implicated in ectopic pregnancy: smoking, being older than 35 or having a previous history of pelvic inflammatory disease.
This group with risk factors should be able to recognize symptoms of ectopic pregnancy and seek immediate medical attention whenever these symptoms arise.
Assisted reproductive techniques (ART):
Some methods of ART, like F, increase the risk marginally. However, it’s noteworthy that the overall risk of ectopic pregnancy after ART remains low. Hence, ART patients should follow their doctors strictly and look out for any signs of ectopic pregnancy.
Smoking:
Decreases motility of the fallopian tube. This could increase the chance of ectopic implantation of the egg. Smokers should, therefore, quit to reduce their risk of ectopic pregnancy.
Symptoms of Ectopic Pregnancy
At first, many symptoms are even similar to the symptoms of a regular pregnancy, thus making it difficult to differentiate. Important features include:
Early symptoms of ectopic pregnancy:
- Missed Period
- Breast Tenderness
- Nausea or Vomiting
Warning signs of an ectopic pregnancy:
- Pelvic or abdominal pain: This is often sharp and quite localized to one side.
- Vaginal spotting or bleeding: This can be light or heavy and is often mistaken for an irregular period.
- Pain at shoulder tip: Internal bleeding irritates the diaphragm.
- Dizziness or fainting: Suggests significant blood loss or shock.
Diagnostic Methods for Early Detection
The early detection of ectopic pregnancy requires a combination of clinical evaluation, laboratory tests, and imaging techniques.
1. Clinical Evaluation
A proper history and physical examination lay the groundwork for the diagnosis:
Medical History:
Risk factors such as previous ectopic pregnancy, infections, or tubal surgeries are evaluated.
Pelvic Examination:
Note any tenderness, masses, or any cervical motion tenderness.
2. Laboratory tests
Human Chorionic Gonadotropin (hCG):
In ectopic pregnancies, hCG concentrations are lower than expected. Serial hCG testing (every 48 hours) has been used to determine whether levels rise abnormally or plateau.
Progesterone Levels:
In cases of hCG <5 ng/mL, this indicates a non-existent pregnancy or a possible ectopic pregnancy.
3. Imaging Techniques
Transvaginal Ultrasound (TVUS):
This is the definitive test for the diagnosis of ectopic pregnancy. In the instance of a diagnosis, the absence of an intrauterine pregnancy with hCG ≥ 1,500-2000 mIU/mL renders the condition suspicious (discriminatory zone). The ultrasound is also indicated to demonstrate an adnexal mass, or free fluid in the pelvis.
Doppler Ultrasound:
Will show blood flow in an area of suspected ectopic pregnancy.
MRI or CT Scan:
Only rarely utilized for patients with exceptional cases, such as abdominal pregnancies.
4. Minimally Invasive Techniques
Diagnostic Laparoscopy:
A definitive method for diagnosis. Direct visualization of the ectopic pregnancy.
Modern Advances in Early Detection
These rapid tests for hCG allow fast assessment in emergency settings.
Biomarkers Other Than hCG:
Currently being investigated by researchers are possible alternative markers-Creatine Kinase and ADAM-12- aimed at providing an improved diagnosis.
Artificial Intelligence (AI):
AI-assisted ultrasound systems hold promise for early diagnosis of ectopic pregnancies.
Differential Diagnosis
Ectopic pregnancy symptoms overlap with other conditions. Differential diagnosis includes:
- Miscarriage: Early pregnancy loss with heavy bleeding and cramping.
- Ovarian cyst rupture: Sudden onset of pelvic pain.
- Pelvic inflammatory disease (PID): Pain with fever and discharge.
- Appendicitis: Right lower abdominal pain with nausea or fever.
Management of Ectopic Pregnancy
Management can occur if early diagnosis is made; however, the type of approach is dependent on the condition of the patient, the level of hCG, and the size and location of the ectopic pregnancy.
1. Medical Management:
Methotrexate Therapy:
A folate antagonist that inhibits cell division within the ectopic pregnancy. Indicated for stable patients with low hCG levels (<5,000 mIU/mL). Methotrexate therapy is contraindicated in patients with renal or hepatic dysfunction, active pulmonary disease, or immunodeficiency. Close monitoring of hCG levels after treatment is essential to ensure the ectopic pregnancy has resolved.
2. Surgical Management:
Laparoscopic Salpingectomy/Salpingostomy:
Removal of the ectopic pregnancy or affected fallopian tube. Preferred operative procedure in instances of ruptured ectopic pregnancy or unstable patient.
There are situations in which surgical management becomes necessary, for example, when a patient is not a candidate for medical therapy or manifests severe symptoms. Laparoscopic methods are minimally invasive and associated with fewer complications than open surgery.
Open Surgery (Laparotomy):
Reserved for emergencies or when laparoscopic expertise is unavailable. Open surgery, that is laparotomy, is usually reserved for instances in which a severe ectopic pregnancy needs immediate intervention.
This mode of therapy may be adopted in the case of emergencies or when laparoscopic expertise is not readily available.
3. Expectant Management:
In selected instances, small ectopic pregnancies resolve spontaneously, meaning they require no intervention.
Expectant management will include close observation of the patient’s condition to see whether the ectopic pregnancy resolves spontaneously without the need for surgical intervention. This is generally an approach for small ectopic pregnancies that have a low risk of complications.
Preventing Ectopic Pregnancy
Although prevention is not possible in all situations, risk can be reduced by certain means:
- Treat infections on time: prevent tubal scarring.
- Avoid smoking: Tubal health is improved.
- Go for gynaecological check-ups: Early detection of abnormalities.
- Use ART responsibly: Avoid complications.
Importance of Regular Follow-Up
Patients treated for ectopic pregnancy must be kept under close follow-up to check on their hCG levels until the levels fall to zero. This ensures complete resolution of the ectopic pregnancy and minimizes the chances of recurrence.
Further regular monitoring of hCG levels also allows for the early detection of any complications so that they can be promptly intervened on if required. The welfare of patients post-treatment is an important aspect of care that needs strict monitoring by healthcare providers to prevent complications that might arise in the future.
Conclusion
Timely diagnosis of ectopic pregnancy is indispensable to protect maternal health and fertility. The appearance of symptoms, appropriate use of diagnostic aids, and awareness of risk factors are the essential steps that ensure quick intervention.
Symptoms of ectopic pregnancy include abdominal pain, survival bleeding, and shoulder pain. If an ectopic pregnancy is not managed well, it can lead to life-threatening complications such as internal bleeding and rupture of the fallopian tube.
For people and couples who try to find treatments for infertility issues, comprehensive reproductive health becomes important. This is where centres like Nimaaya act as a guiding light, with patient empowerment being their main focus through offering expert care and direction, nurturing hope, and helping patients in their reproductive decisions.