The significance of prenatal screening tests in obstetrics lies in assisting parents-to-be and healthcare workers to make crucial decisions regarding the health of the fetus. Among these biochemical methods to screen for chromosomal aberrations-down syndrome (Trisomy 21), Edwards syndrome (Trisomy 18), and Neural Tube Defects (NTDs)-are the Double Marker Test vs the Triple Marker Test.
While both tests intend to serve similar purposes, they differ in their timing, type of biomarkers analyzed, and clinical application. Any obstetrician, gynecologist, fertility specialist, or even expecting parents must understand these differences.
An Explanation of Prenatal Screening
Prenatal screening tests are meant to detect the possibility, not to diagnose certain genetic conditions; they thus serve a predictive value. These are non-invasive, and either a blood test or ultrasound is done, or sometimes both are done. The screening tests are contrasted with the diagnostic tests performed during pregnancy, such as amniocentesis or CVS, which provide almost sure confirmation of abnormalities but bear a risk of miscarriage.
Depending on the stage of pregnancy at which they are performed, and the biochemical markers studied, the Double Marker Test and the Triple Marker Test fall under the broad category of maternal serum screening tests.
Double Marker Test: An Overview

What Is It?
Being done in the first trimester, the Double Marker Test is a screening test combining assessment of:
- Free Beta-human Chorionic Gonadotropin (β-hCG)
- Pregnancy-Associated Plasma Protein-A (PAPP-A)
These markers are evaluated in conjunction with a nuchal translucency (NT) ultrasound measurement, which assesses the thickness at the back of the fetal neck.
Timing
- Conducted between 11 to 13 weeks of gestation (ideally before 13 weeks + 6 days).
Purpose
The Double Marker Test helps assess the risk of the fetus having chromosomal conditions such as:
- Down syndrome (Trisomy 21)
- Edwards syndrome (Trisomy 18)
- Patau syndrome (Trisomy 13)
Procedure
- A blood sample is taken from the mother.
- An NT scan is performed by a sonographer.
- Combined data is analyzed using software algorithms that incorporate:
- Maternal age
- Weight
- Ethnicity
- Gestational age
- Biomarker levels
- NT measurement
Interpretation
Results are reported as:
- Low Risk: Risk is minimal; no further testing is usually required.
- High Risk: Indicates a higher likelihood of chromosomal abnormality; further diagnostic testing is recommended.
Accuracy
- Detection rate of Down syndrome: ~85%
- False positive rate: ~5%
Advantages
- Early detection enables better management.
- More accurate when combined with NT scan.
- Non-invasive and safe for both mother and fetus..
Know More:डबल मार्कर टेस्ट की रिपोर्ट को कैसे समझें?
Triple Marker Test: Overview
What Is It?

The Triple Marker Test (also known as Triple Screen Test) is a second-trimester screening test that measures three different substances in the mother’s blood:
- Alpha-fetoprotein (AFP)
- Beta-hCG
- Unconjugated Estriol (uE3)
Sometimes, a Quadruple Marker Test adds Inhibin A for greater accuracy.
Timing
- Performed between 15 to 20 weeks of gestation (ideally between 16-18 weeks).
Purpose
The test evaluates the risk of:
- Neural tube defects (e.g., spina bifida, anencephaly)
- Down syndrome (Trisomy 21)
- Edwards syndrome (Trisomy 18)
Procedure
- Maternal blood sample is collected.
- Lab evaluates the levels of AFP, β-hCG, and uE3.
- Risk is calculated using a formula that considers:
- Maternal age
- Weight
- Race
- Diabetic status
- Gestational age
Interpretation
- High AFP: Suggests a possible neural tube defect or incorrect gestational dating.
- Low AFP, high hCG, low uE3: Increased risk for Down syndrome.
- Low AFP, low hCG, low uE3: Suggests Edwards syndrome.
Accuracy
- Detection rate for Down syndrome: ~70%
- Neural tube defect detection: ~85-90%
Advantages
- Useful when a first-trimester test (like the Double Marker) is missed.
- Can screen for neural tube defects, which the Double Marker test does not.
Key Differences: Double Marker Test vs Triple Marker Test
| Criteria | Double Marker Test | Triple Marker Test |
| Timing | 11–13+6 weeks (1st trimester) | 15–20 weeks (2nd trimester) |
| Markers Evaluated | β-hCG, PAPP-A | AFP, β-hCG, uE3 |
| Additional Test Required | NT scan | No NT scan required |
| Detection of Neural Tube Defects | No | Yes |
| Accuracy for Down Syndrome | ~85% | ~70% |
| Test Type | Combined screening (biochemical + ultrasound) | Biochemical only |
| Fetal Abnormalities Detected | Trisomy 21, 18, 13 | Trisomy 21, 18, Neural tube defects |
| Best Use Case | Early risk assessment, if early prenatal care available | If patient missed 1st trimester screening |
| Procedure | Blood draw + NT scan | Blood draw only |
| Invasiveness | Non-invasive | Non-invasive |
Clinical Significance
Both tests play important roles in the early detection of chromosomal abnormalities, allowing parents time to consider diagnostic testing and plan for medical or emotional support.
- Double Marker Test is often the preferred choice due to its early timing and higher accuracy, especially when coupled with an NT scan.
- Triple Marker Test is useful when the patient seeks care later or when there is a need to evaluate neural tube defects.
Importantly, neither test is diagnostic. A “high-risk” result only indicates an increased probability, not a definitive outcome. Such results should always be followed up with diagnostic tests like:
-
- Non-Invasive Prenatal Testing (NIPT)
- Amniocentesis
- Chorionic Villus Sampling (CVS)
Risk Factors That Influence Test Results
- Maternal age >35 years
- Family history of chromosomal disorders
- Previous pregnancies with anomalies
- Diabetes or certain medications (e.g., anticonvulsants)
- Obesity or incorrect gestational dating
These factors are incorporated into the risk algorithm to improve result accuracy.
Role in Assisted Reproductive Technology (ART)
For patients undergoing IVF or other assisted reproductive techniques, these tests take on increased importance because:
- Advanced maternal age is more common.
- Multiple pregnancies may complicate interpretation.
- Ensuring fetal well-being is paramount given the emotional and financial investment.
In such cases, fertility centers like Nimaaya IVF provide comprehensive prenatal counseling that includes selecting the appropriate test based on gestational age, health history, and treatment protocol.
Challenges and Limitations
- False positives/negatives can cause anxiety or provide false reassurance.
- Limited accuracy compared to advanced methods like NIPT or genetic testing.
- Requires accurate gestational dating to ensure result reliability.
- Sometimes, test results are inconclusive due to lab or biological variability.
Thus, informed consent, genetic counseling, and a clear explanation of test limitations are essential components of prenatal care.
Integration With NIPT and Diagnostic Testing
While Double and Triple Marker Tests are common, many clinicians are now moving toward Non-Invasive Prenatal Testing (NIPT), especially for high-risk pregnancies. NIPT has a detection rate of over 99% for Down syndrome and is done as early as 10 weeks.
However, cost and accessibility remain barriers in many regions, making Double and Triple Marker Tests valuable, especially in resource-limited settings.
Choosing Between Double Marker Test and Triple Marker test
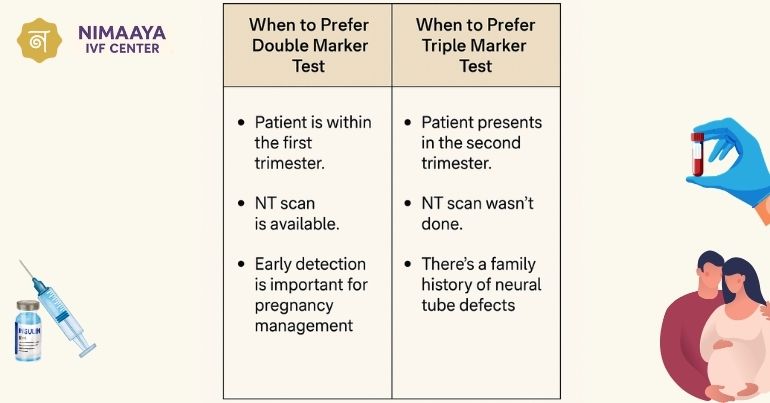
When to Prefer Double Marker Test:
- Patient is within the first trimester.
- NT scan is available.
- Early detection is important for pregnancy management.
When to Prefer Triple Marker Test:
- Patient presents in the second trimester.
- NT scan wasn’t done.
- There’s a family history of neural tube defects.
Sometimes, both tests may be used in a sequential screening approach, enhancing diagnostic accuracy.
Conclusion
Prenatal screening is an evolving landscape that empowers families to prepare for all possibilities in a pregnancy. The Double Marker Test, with its early timing and higher accuracy, is often the first line of defense in prenatal care. On the other hand, the Triple Marker Test remains a valuable second-trimester option, especially when early screening is missed or if neural tube defects are a concern.
Choosing the right test depends on timing, clinical history, and availability. Both tests are non-invasive, safe, and offer crucial insights into fetal development. However, abnormal results should always be followed up with diagnostic procedures and genetic counseling to confirm findings.
At the forefront of advanced reproductive healthcare, Nimaaya IVF Center in India plays a pivotal role in supporting expectant parents through every phase of their journey—from conception to delivery. With state-of-the-art technology, compassionate care, and a focus on personalized medicine, Nimaaya ensures that prenatal screening decisions are made with clarity and confidence.
FAQ
Can I do both the Double Marker and Triple Marker Test?
Yes, both tests can be performed sequentially. This is sometimes done to increase the overall accuracy of screening or if there is uncertainty or late presentation during pregnancy.
Which test is more accurate for detecting Down syndrome?
The Double Marker Test combined with an NT scan is more accurate, with a detection rate of around 85%, while the Triple Marker Test has a detection rate of around 70% for Down syndrome.
What happens if my test result is “high risk”?
A “high-risk” result does not confirm a problem. It means there’s a higher probability of a chromosomal abnormality. In such cases, your doctor may recommend diagnostic tests like amniocentesis, chorionic villus sampling (CVS), or Non-Invasive Prenatal Testing (NIPT) for confirmation.