Introduction
The inability to conceive is known as infertility. Healthcare providers diagnose after a couple has had unprotected intercourse for a full year without becoming pregnant. Treatment options for infertility include hormone-correcting medications, surgery, and other reproductive procedures, in addition to IVF. We will go into depth about treatment options, risk factors, common causes of female infertility, and more in this guide.
What is Female Infertility?
A medical condition called infertility prevents a person from becoming pregnant. It is a challenge you face if you’re younger than 35 and haven’t been able to get pregnant after trying for one year.
If you’re older than 35 and haven’t conceived after more than 6 months if you’ve lost two or more pregnancies to miscarriage, or if you have tried other fertility treatments without results. When you are trying to conceive, you are engaging in regular, birth control-free sex. A person may receive an earlier diagnosis if they have another medical condition, such as uterine factor infertility.
Causes of infertility can be due to either partner. The male reproductive system will fail similarly as frequently as the female reproductive system can, leading to infertility. Causes of female infertility are mainly by age, hormonal imbalances, illnesses, changes in lifestyle, or environmental factors.
Healthcare experts refer to infertility as a “female factor” or “female infertility” when the cause is thought to come from a person with a uterus. You should seek help sooner if you have irregular menstrual cycles or have had gynecological issues such as endometriosis, pelvic surgery, tubal pregnancies, or infections.
Also Read: Female Infertility: Causes, Diagnosis, and Treatment Options
Types of Infertility in Females
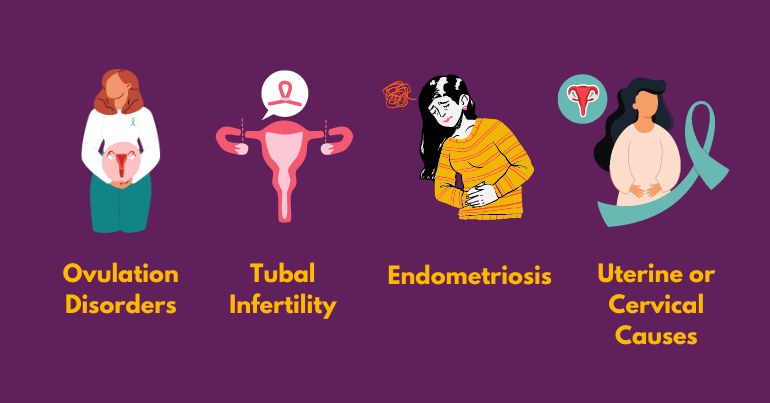
There are mainly four main causes of female infertility. Let’s get in more detail:
❧ Ovulation Disorders
One of the most common causes of female infertility in females is infrequent ovulation or the complete absence of it. This disorder is caused by irregular reproductive hormone production by the hypothalamus or pituitary gland. Ovulation disorders can take many forms, like,
- Polycystic Ovary Syndrome (PCOS) causes hormone imbalances, resulting in ovulation disorders. It is considered one of the most common causes of female infertility and can be caused by insulin resistance, obesity, excessive or abnormal facial hair growth, and acne.
- Hypothalamic Dysfunction: Follicle-stimulating hormone (FSH) and Luteinizing Hormone (LH) cause women to ovulate every month. The secretion of these hormones may be adversely affected due to excess emotional, physical, or mental stress or sudden weight loss or gain. Such a condition manifests through irregular or missed periods.
- Premature Ovarian Failure: This anomaly, often referred to as primary ovarian insufficiency, is brought on by an inflammatory reaction or the unexpected or early loss of eggs as a result of chemotherapy or heredity.
- High Prolactin: Infertility can result from the pituitary gland producing excessive amounts of prolactin, which lowers the generation of estrogen.
❧ Tubal Infertility
The fallopian tubes may be damaged, blocking an egg from entering them and leading to tubal infertility. Blocked or damaged fallopian tubes can be due to:
- A pelvic inflammatory disease infects the fallopian tubes and uterus through gonorrhea or STIs (sexually transmitted infections).
- Past surgeries in the pelvis or abdomen
❧ Endometriosis
This type of infertility in females occurs when uterine tissues start growing outside the uterus. In some situations, it is possible to surgically remove the excess tissue, although doing so may leave scars that obstruct the fallopian tubes. Endometriosis can damage a fertilized egg.
❧ Uterine or Cervical Causes
Sometimes the cause of infertility in females can be cervical or uterine, which can prevent egg implantation or even result in a miscarriage. These causes can take various forms, such as:
- Fibroids (myomas) are common in the uterus.
- An unusually shaped uterus
- Cervical stenosis that narrows the cervix area
- Inability to produce mucus from the cervix to allow easy travel of the sperm into the uterus
Also Read: A Comprehensive Guide to Cervical Cancer
Risk Factors for Female Infertility
Many factors can increase your risk of infertility. General health conditions, genetic (inherited) traits, lifestyle choices, and age can all contribute to infertility. Specific factors can include:
- Age. Generally, fertility starts to decline in your 30s.
- Hormone issues that prevent ovulation.
- Abnormal menstrual cycle.
- Obesity.
- Having underweight.
- Overexercise or intense exercise.
- Endometriosis.
- Structural problems (medical issues about your ovaries, uterus, or fallopian tubes).
- Uterine fibroids.
- Ovarian cysts.
- Tumors.
- Autoimmune disorders (lupus, rheumatoid arthritis, Hashimoto’s disease).
- Sexually transmitted infections (STIs) cause pelvic inflammatory disease.
- Polycystic ovary syndrome (PCOS).
- Primary ovary insufficiency (POI).
- Smoking.
- A past ectopic pregnancy.
Can Female Infertility Be Prevented?
You can’t predict or prevent most types of female infertility. With lifestyle changes, you could be able to manage a few of the risk factors that lead to infertility. Examples include:
- Reducing alcohol consumption.
- Quitting smoking.
- Maintaining a healthy weight for you.
- Developing a good exercise routine.
- Eating a healthy diet rich in fruits and vegetables.
- Sleep for at least seven hours at night
It’s important to regularly visit your healthcare provider and discuss any other risks you may have for infertility. Once you start having sex, you should also plan yearly examinations with a gynecologist so that your medical professional can more accurately identify any issues that may impact your future fertility.
Diagnosis and Tests
Diagnostic procedures can identify the causes of infertility. Other times, pinpointing the cause requires time and patience. And, in some cases, no cause of infertility can be found.
Often, a complete medical history and physical examination precede a diagnostic evaluation. Afterwards, the physician may further evaluate using one or more of the following methods:
- Confirming ovulation
- Conducting a blood test: To find out if there is proper ovulation physiology, a blood test will be performed. Structural abnormalities and age-related factors can all cause ovulation failure.
- Assessing ovarian reserve: A physician evaluates the follicle-stimulating hormone (FSH) level. To ascertain the quantity and quality of eggs that remain in a woman’s ovary, a blood test is conducted.
- Measuring hormone levels: A common cause of infertility is polycystic ovary syndrome (PCOS). This syndrome is genetically linked to hormonal imbalances thereby causing a condition that prevents ovulation.
- Performing a post-coital test: To determine how effectively sperm survive in a woman’s reproductive tract, the cervical mucus is examined after sexual activity.
- Taking a biopsy of the endometrium (lining of the uterus): This test further investigates problems with ovulation or hormones.
Depending on the patient’s condition, additional detailed tests may be performed to determine the cause of the infertility.
Female Infertility Treatment
❧ Hormone Therapy to Induce Ovulation
Medications may be used to induce ovulation in those who are not ovulating or are ovulating irregularly. Hormone treatment can also be used to treat other disorders related to the endocrine system, which produces hormones.
The causes of ovulation failure are numerous. Polycystic ovarian syndrome (PCOS) is the most common cause.
❧ In Vitro Fertilization
When the fallopian tubes are badly damaged or nonexistent, or when infertility is due to male factors, in vitro fertilization (IVF) is the recommended or most common treatment for infertility. IVF has been utilized more often as a first line of therapy for all reasons of infertility in recent years because of its high success rate.
When carrying out in vitro fertilization, the following procedures are followed:
- Multiple follicles carrying eggs are stimulated to develop from the ovaries.
- The advancement of follicular growth is monitored by measuring hormone levels and using ultrasounds when necessary.
- The retrieval of the eggs is guided by a transvaginal ultrasound.
- As soon as possible, the recovered eggs are brought to the lab to be fertilized and cultivated.
- The developing pre-embryos are placed into the uterus on a prearranged date.
These procedures involve a variety of carefully choreographed procedures to ensure the best success.
❧ Surgical Options
Adhesions, or scar tissue, and endometriosis are surgically removed when they obstruct the fallopian tube or impair its ability to receive an egg. Our capacity to accomplish this has increased thanks to advanced techniques, which frequently involve non-invasive laparoscopic procedures or microsurgical procedures to repair the uterus or fallopian tubes. Without the need for in vitro fertilization, microsurgical repair is a viable alternative for reversing tubal sterilization and frequently yields good results. The quickest method is in vitro fertilization when the fallopian tubes are severely damaged or when it is doubtful that they will respond to surgery.
If there is extensive tubal damage, the affected fallopian tube is usually removed before proceeding to IVF. This helps to achieve greater success for the IVF procedure. For endometriosis, the laparoscopic approach with laser treatment is often effective.
❧ Intrauterine Insemination (IUI)
Intrauterine insemination (IUI) and ovulation induction can be combined. IUI is a relatively “low-tech” assisted reproductive technology (ART) in which cleaned sperm is transferred into the uterus and fallopian tubes, where fertilization occurs. Furthermore, this procedure avoids aggressive cervical mucus and helps resolve issues with motility and sperm count.
❧ Egg Donation
In rare cases with premature ovarian failure, the ovary is no longer releasing eggs because the supply of eggs has been exhausted. Although no treatment is available to reverse this process, it is important to recognize this condition.
When the patient is unable to produce a pregnancy with her eggs, the use of donor eggs can be considered as an option.
Conclusion
Infertility can be incredibly stressful. If you’ve been trying to get pregnant for 12 months without success — or six months if you’re over the age of 35. The goal of Nimaaya IVF Center is to assist couples in realizing their goal of becoming parents by successfully increasing fertility rates. Our team of experienced fertility specialists will work with you to create a personalized treatment plan that fits your unique needs. With cutting-edge technology and compassionate care, we are dedicated to supporting you on your journey to parenthood.