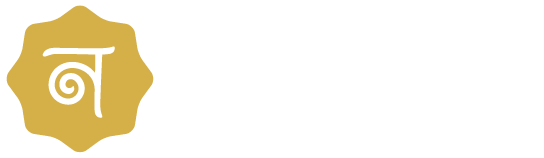
In vitro fertilization (IVF) has revolutionized the field of reproductive medicine and has helped countless couples achieve their dream of parenthood. However, understanding the success rates of IVF can be complex due to the multitude of factors that can influence the outcome. This comprehensive guide aims to provide a clear understanding of IVF success rates, the factors that influence them, and how they are calculated.
Understanding IVF Success Rates
The success rate of IVF is typically defined as the percentage of all IVF procedures that result in a live birth. This rate can vary widely depending on a variety of factors, including the age and health of the patient, the cause of infertility, the quality of the embryos, and the expertise of the clinic.
1. Age and IVF Success Rates
Age is one of the most significant factors affecting IVF success rates. As a woman ages, the quality and quantity of her eggs decline, which can make it more difficult to achieve a successful pregnancy. According to the Society for Assisted Reproductive Technology (SART), the average IVF success rate for women under 35 is around 40%, but this rate declines to around 4% for women over 42.
2. Cause of Infertility and IVF Success Rates
The underlying cause of infertility can also impact IVF success rates. Certain conditions, such as severe male factor infertility or diminished ovarian reserve, may have lower success rates compared to other causes of infertility.
3. Embryo Quality and IVF Success Rates
The quality of the embryos used in IVF can significantly impact success rates. High-quality embryos have a higher chance of implanting and leading to a successful pregnancy. Embryo quality is assessed by embryologists in the lab based on several criteria, including the rate of cell division and the appearance of the cells.
4. Clinic Expertise and IVF Success Rates
The expertise and experience of the fertility clinic and its staff can also influence IVF success rates. Clinics with more experience and advanced technology may have higher success rates due to their expertise in embryo transfer techniques, laboratory protocols, and patient care.
5. Use of Donor Eggs and IVF Success Rates

The use of donor eggs can significantly increase the chances of IVF success, particularly for women who are older or who have poor egg quality. Donor eggs are typically from younger women, which increases the likelihood of successful fertilization and implantation. According to the Centers for Disease Control and Prevention (CDC), the live birth rate for IVF cycles using fresh embryos from donor eggs is approximately 50%.
6. Lifestyle Factors and IVF Success Rates
Lifestyle factors such as smoking, alcohol consumption, and body weight can also impact IVF success rates. Smoking has been shown to reduce the success rates of IVF, while moderate alcohol consumption does not appear to affect IVF outcomes significantly. However, heavy alcohol consumption is discouraged. Obesity has been associated with lower success rates in IVF, likely due to its effects on hormone balance and egg quality.
Interpreting IVF Success Rates
While IVF success rates can provide valuable information, it’s important to interpret them with caution. These rates are averages and may not reflect an individual’s chances of success. It’s also important to note that a single IVF cycle may not result in a successful pregnancy, and many patients require multiple cycles to achieve a live birth.
1. Fresh vs. Frozen Embryo Transfer Success Rates
Success rates can vary depending on whether fresh or frozen embryos are used. Some studies have shown that frozen embryo transfers (FET) may have slightly higher success rates compared to fresh transfers. This may be due to the ability to transfer the embryos in a more natural hormonal environment in FET cycles.
2. Single vs. Multiple Embryo Transfer Success Rates
The number of embryos transferred can also impact success rates. Transferring multiple embryos may increase the chances of pregnancy, but it also increases the risk of multiple pregnancies, which can pose risks to both the mother and the babies. As a result, many clinics now advocate for single embryo transfer (SET) to reduce these risks.
3. Cumulative IVF Success Rates
Cumulative success rates refer to the success rates over multiple IVF cycles. These rates are often higher than the success rates for a single cycle, as they take into account the cumulative effect of multiple attempts.
4. Success Rates by Diagnosis
IVF success rates can also vary depending on the cause of infertility. For instance, women with polycystic ovary syndrome (PCOS) often respond well to the stimulation of the ovaries used in IVF, leading to higher success rates. On the other hand, women with low ovarian reserves may have lower success rates because they produce fewer eggs.
5. Success Rates by Treatment Protocol
Different treatment protocols can also impact IVF success rates. For instance, some studies have found that the use of intracytoplasmic sperm injection (ICSI) can improve success rates in cases of severe male factor infertility. The use of preimplantation genetic testing (PGT) can also increase success rates by ensuring that only genetically normal embryos are transferred.
6. Success Rates by Clinic
Success rates can also vary significantly from clinic to clinic. Factors such as the expertise of the medical team, the quality of the lab, and the specific treatments and protocols used can all impact success rates. It’s important to research and choose a clinic that has high success rates and a good reputation for patient care.
The Role of Individualized Treatment in Improving IVF Success Rates
At Nimaaya, we believe that individualized treatment is key to improving IVF success rates. Our team of experienced fertility specialists takes the time to understand each patient’s unique situation and tailor treatment accordingly.
1. Personalized Treatment Plans
We create personalized treatment plans based on a thorough evaluation of each patient’s medical history, age, cause of infertility, and personal preferences. This allows us to optimize each step of the IVF process, from ovarian stimulation to embryo transfer, to maximize the chances of success.
2. Advanced Laboratory Techniques
Our state-of-the-art laboratory uses advanced techniques to improve IVF outcomes. This includes ICSI for cases of male factor infertility, blastocyst culture to select the best quality embryos, and PGT to screen for genetic abnormalities.
3. Comprehensive Care
We provide comprehensive care that addresses both the physical and emotional aspects of IVF. Our team includes fertility specialists, embryologists, nurses, and counselors who work together to provide the best possible care. We also offer support services such as nutrition counseling, acupuncture, and mind-body programs to enhance overall well-being and improve IVF outcomes.
Conclusion
Understanding IVF success rates can be complex, but they are an important part of the decision-making process for couples considering IVF. At Nimaaya IVF Center, we are committed to providing clear, accurate information and personalized care to help our patients achieve their dream of parenthood. We believe that with the right support and treatment, many couples can overcome infertility and build the family they’ve always dreamed of.